This year’s HRS is going to be one to remember! We are proud to present late breaking data and product advancements for the Amplatzer™ Amulet™ Left Atrial Appendage Occluder. We have made it easy to SAVE THE DATE below, by adding it to your calendar with a click.
Calendar
Fri Apr 25
Sat Apr 26
MAT-2502878 v1.0
CLOSURE. ONCE AND FOR ALL.1,2
We strive to create a passionate community of physicians who not only understand why their patients deserve the life-changing benefits of Amulet but also feel a profound sense of belonging to a global community of Amulet implanters.
Amplatzer™ Amulet™ LAA Occluder
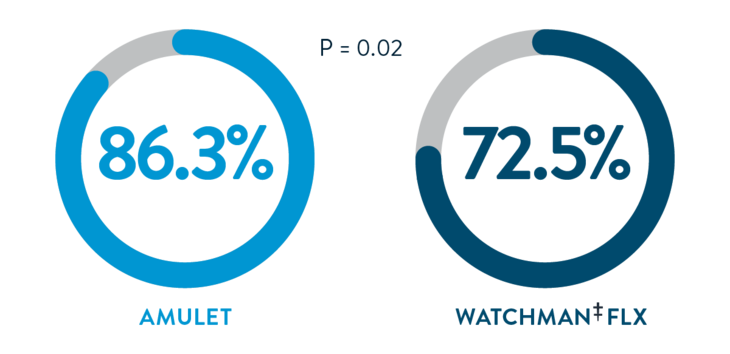
Amulet IDE closure at 12 months3
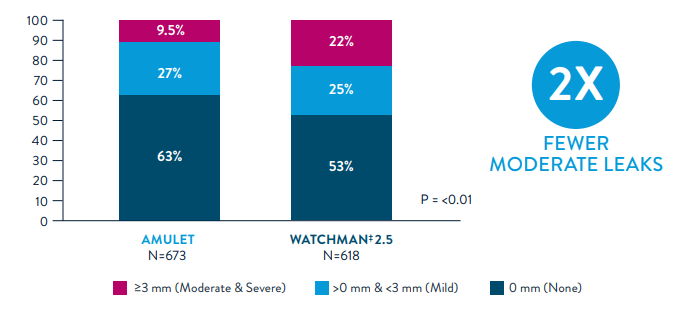
Swiss-Apero Complete Closure At 45 Days By TEE4
Significantly Higher Complete Closure


Resources for Your Patients
Abbott Cardiovascular supports you with all aspects of patient care. Please find resources to use with your patients.
A Patient’s Guide To The Nonsurgical Closure Of The Left Atrial Appendage
AMPLATZER™ AMULET™ LEFT ATRIAL APPENDAGE OCCLUDER
Important Safety Information
INDICATION FOR USE
The Amplatzer™ Amulet™ Left Atrial Appendage Occluder is a percutaneous transcatheter device intended to reduce the risk of thrombus embolization from the left atrial appendage (LAA) in patients who have nonvalvular atrial fibrillation and who are at increased risk for stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores, are suitable for short term anticoagulation therapy, and have appropriate rationale to seek a non-pharmacologic alternative to oral anticoagulation, taking into consideration the safety and effectiveness of the device.
CONTRAINDICATIONS
The Amplatzer™ Amulet™ Left Atrial Appendage (LAA) Occluder is contraindicated for patients:
- With the presence of intracardiac thrombus.
- With active endocarditis or other infections producing bacteremia.
- Where placement of the device would interfere with any intracardiac or intravascular structures.
POTENTIAL ADVERSE EVENTS
Potential adverse events associated with the device or implant procedure include, but are not limited to, the following: Air embolism; Airway trauma; Allergic reaction; Anemia; Anesthesia reaction (nausea, vasovagal reaction, confusion/altered mental status or other); Arrhythmia; Atrial septal defect; Bleeding; Cardiac arrest; Cardiac tamponade; Chest pain/discomfort; Congestive heart failure; Death; Device embolization; Device erosion; Device malfunction; Device malposition; Device migration; Device-related thrombus; Fever; Hematuria; Hypertension/hypotension; Infection; Multi-organ failure; Myocardial infarction; Perforation; Pericardial effusion; Pleural effusion; Renal failure/dysfunction; Respiratory failure; Seizure; Significant residual flow; Stroke; Thrombocytopenia; Thromboembolism: peripheral and pulmonary; Thrombus formation; Transient ischemic attack; Valvular regurgitation/insufficiency; Vascular access site injury (hematoma, pseudoaneurysm, arteriovenous fistula, groin pain or other); Vessel trauma/injury.
REFERENCES
- Piayda et al., Safety and feasiblity of peri-device leakage closure after LAAO. Eurointervention. 2022.
- Data on file at Abbott
- Ellis et al., Incidence and Clinical Outcomes of Peri-Device Leak After Transcatheter LAAO. HRS. 2022.
- Galea et al. Amulet or Watchman Device for Percutaneous Left Atrial Appendage Closure: Primary Results of the SWISSAPERO Randomized Clinical Trial. Circulation 2022 145:724-738.
